¶ Chronic Inflammation
¶ Summary
Chronic inflammation, also known as "inflammaging," represents a state of persistent, low-grade inflammatory activity that develops with aging. Unlike acute inflammation which is beneficial and self-resolving, chronic inflammation is detrimental and contributes to tissue damage, organ dysfunction, and the development of age-related diseases including cardiovascular disease, neurodegeneration, cancer, and metabolic disorders.
¶ Definition and Overview
¶ Inflammation Types
- Acute inflammation: Rapid, beneficial response to injury or infection
- Chronic inflammation: Persistent, low-grade inflammatory state
- Sterile inflammation: Tissue damage without infectious agents
- Neuroinflammation: Brain-specific inflammatory processes
- Metaflammation: Metabolic tissue inflammation
¶ Inflammaging Characteristics
- Persistent cytokine elevation: Sustained pro-inflammatory mediator production
- Failed resolution: Impaired return to homeostatic state
- Tissue damage: Progressive organ dysfunction and pathology
- Systemic effects: Multi-organ involvement and disease susceptibility
- Self-perpetuating: Inflammation causing further inflammatory triggers
¶ Molecular Mechanisms of Chronic Inflammation
¶ Pro-inflammatory Mediators
- Interleukin-1β (IL-1β): Potent inflammatory cytokine and fever inducer
- Interleukin-6 (IL-6): Multi-functional cytokine affecting multiple systems
- Tumor necrosis factor-α (TNF-α): Major inflammatory mediator and cell death inducer
- Interferon-γ (IFN-γ): Th1 immune response activator
- Chemokines: CCL2, CXCL1, CXCL8 directing immune cell recruitment
¶ Transcriptional Control
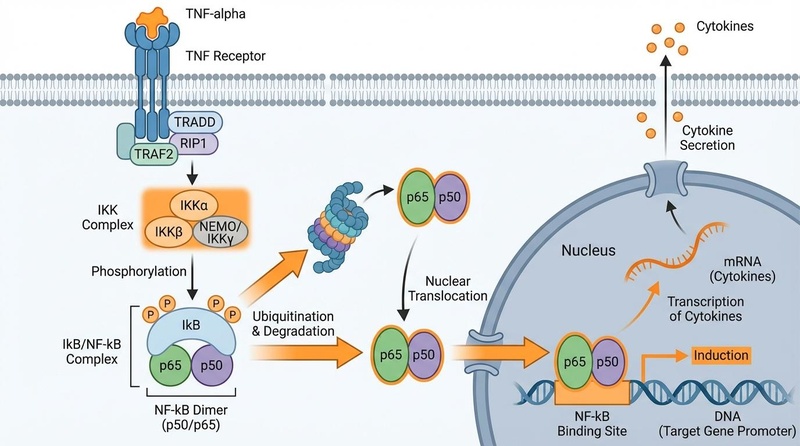
Schematic representation of the NF-κB signaling pathway, a master regulator of inflammation.
- NF-κB pathway: Master regulator of inflammatory gene expression
- AP-1 transcription factors: Jun and Fos family inflammatory regulators
- IRF family: Interferon regulatory factors controlling immune responses
- STAT signaling: Signal transducers and activators of transcription
- C/EBP factors: CCAAT/enhancer-binding proteins in inflammation
¶ Pattern Recognition Receptors
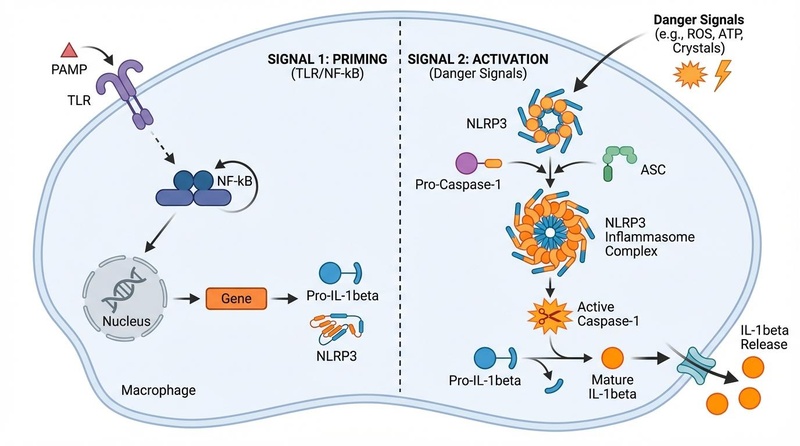
Mechanism of NLRP3 inflammasome activation involving priming and activation steps.
- Toll-like receptors (TLRs): Pathogen and damage recognition
- NLRP3 inflammasome: Cytoplasmic danger signal detection
- cGAS-STING pathway: Cytosolic DNA sensing and response
- RIG-I-like receptors: Viral RNA detection and signaling
- Complement system: Classical, alternative, and lectin pathways
¶ Sources of Chronic Inflammation
¶ Cellular Senescence
- Senescence-associated secretory phenotype (SASP): Inflammatory factor secretion
- p16+ cell accumulation: Age-related senescent cell burden increase
- Tissue dysfunction: Loss of functional cells and inflammatory environment
- Systemic effects: Circulating SASP factors affecting distant tissues
- Therapeutic targets: Senolytic and senomorphic interventions
¶ Damage-Associated Molecular Patterns (DAMPs)
- High mobility group box 1 (HMGB1): Nuclear protein released during damage
- Heat shock proteins: Intracellular chaperones acting as danger signals
- Uric acid: Metabolic waste product triggering inflammation
- ATP: Extracellular nucleotide damage signal
- Mitochondrial DNA: Released mtDNA mimicking bacterial DNA
¶ Oxidative Stress
- Reactive oxygen species (ROS): Superoxide, hydrogen peroxide, hydroxyl radicals
- Reactive nitrogen species (RNS): Nitric oxide, peroxynitrite, nitrogen dioxide
- Antioxidant decline: Reduced superoxide dismutase, catalase, and glutathione
- Mitochondrial dysfunction: Increased ROS production and decreased efficiency
- Lipid peroxidation: Membrane damage and inflammatory lipid mediators
¶ Infectious Agents
- Chronic infections: Cytomegalovirus, Epstein-Barr virus, Helicobacter pylori
- Viral reactivation: Latent virus reactivation in immunosenescence
- Bacterial translocation: Gut permeability and systemic bacterial exposure
- Biofilm formation: Persistent bacterial communities
- Antimicrobial resistance: Treatment-resistant chronic infections
¶ Tissue-Specific Chronic Inflammation
¶ Neuroinflammation
- Microglial activation: Brain-resident immune cell inflammatory responses
- Astrocyte reactivity: Glial cell inflammatory and supportive functions
- Blood-brain barrier dysfunction: Increased permeability and immune infiltration
- Neurodegeneration: Alzheimer's, Parkinson's, and other brain diseases
- Cognitive decline: Inflammation-mediated memory and learning deficits
¶ Vascular Inflammation
- Endothelial dysfunction: Impaired vascular function and regulation
- Atherosclerosis: Inflammatory arterial plaque formation
- Smooth muscle cell activation: Vascular remodeling and stiffness
- Thrombosis risk: Increased blood clotting and cardiovascular events
- Hypertension: Inflammatory mechanisms in blood pressure elevation
¶ Adipose Tissue Inflammation
- Macrophage infiltration: M1 pro-inflammatory macrophage accumulation
- Adipokine dysregulation: Altered leptin, adiponectin, and resistin production
- Insulin resistance: Inflammation-mediated metabolic dysfunction
- Lipolysis increase: Enhanced fat breakdown and free fatty acid release
- Metabolic syndrome: Clustering of inflammatory metabolic risk factors
¶ Muscle Inflammation
- Sarcopenia: Age-related muscle mass and strength loss
- Myokine imbalance: Altered muscle-derived signaling molecules
- Satellite cell dysfunction: Impaired muscle regeneration capacity
- Fibrosis: Excessive collagen deposition and muscle stiffness
- Exercise intolerance: Reduced physical capacity and endurance
¶ Immune System Dysfunction
¶ Immunosenescence
- Thymic involution: Progressive immune organ shrinkage and dysfunction
- T cell exhaustion: Chronic activation and functional decline
- B cell dysfunction: Reduced antibody production and quality
- NK cell changes: Altered natural killer cell function
- Autoimmunity: Increased self-reactive immune responses
¶ Inflammatory Cell Types
- M1 macrophages: Pro-inflammatory, classically activated phenotype
- Th1 and Th17 cells: Pro-inflammatory T helper cell subsets
- Neutrophils: Acute inflammatory cells with chronic activation
- Dendritic cells: Antigen-presenting cells driving immune responses
- Mast cells: Allergic and inflammatory mediator-releasing cells
¶ Resolution Failure
- Specialized pro-resolving mediators (SPMs): Lipoxins, resolvins, protectins, maresins
- Efferocytosis impairment: Reduced clearance of dead cells
- Regulatory T cell dysfunction: Impaired immune suppression
- Anti-inflammatory cytokines: Decreased IL-10, TGF-β production
- Cholinergic anti-inflammatory pathway: Vagal nerve immune modulation decline
¶ Clinical Manifestations
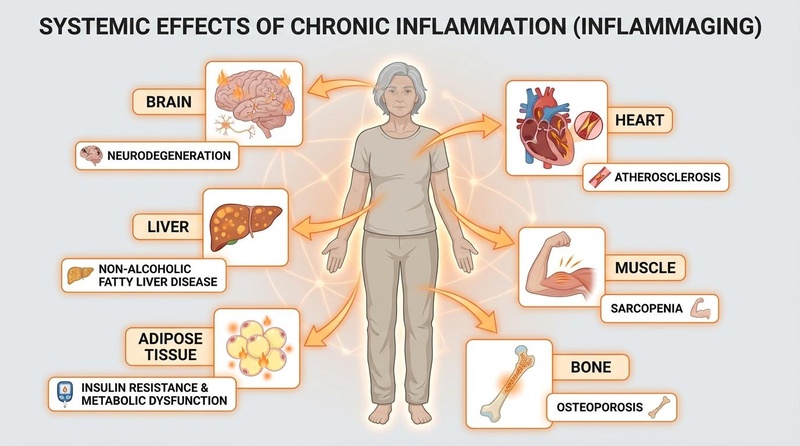
Systemic effects of chronic inflammation (inflammaging) across multiple organ systems.
¶ Cardiovascular Disease
- Coronary artery disease: Inflammatory atherosclerotic plaque formation
- Heart failure: Inflammatory cardiac remodeling and dysfunction
- Stroke: Cerebrovascular inflammation and thrombosis
- Peripheral artery disease: Systemic vascular inflammatory damage
- Arrhythmias: Inflammation-induced electrical conduction abnormalities
¶ Neurological Disorders
- Alzheimer's disease: Neuroinflammation and amyloid pathology
- Parkinson's disease: Microglial activation and dopaminergic neuron loss
- Multiple sclerosis: Autoimmune neuroinflammatory demyelination
- Depression: Inflammatory cytokines affecting mood regulation
- Cognitive decline: Inflammation-mediated memory and executive dysfunction
¶ Metabolic Diseases
- Type 2 diabetes: Inflammatory insulin resistance and β-cell dysfunction
- Obesity: Adipose tissue inflammation and metabolic dysfunction
- Non-alcoholic fatty liver disease: Hepatic inflammation and fibrosis
- Metabolic syndrome: Inflammatory clustering of risk factors
- Gout: Uric acid crystal-induced inflammatory arthritis
¶ Cancer
- Tumor promotion: Inflammatory microenvironment supporting cancer growth
- DNA damage: Inflammation-induced genomic instability
- Angiogenesis: Inflammatory factor-promoted blood vessel formation
- Metastasis: Inflammation facilitating cancer spread
- Immune evasion: Chronic inflammation impairing anti-tumor immunity
¶ Autoimmune Diseases
- Rheumatoid arthritis: Joint inflammation and destruction
- Inflammatory bowel disease: Chronic gut inflammation
- Psoriasis: Skin inflammatory autoimmune condition
- Systemic lupus erythematosus: Multi-organ autoimmune inflammation
- Vasculitis: Blood vessel inflammatory diseases
¶ Detection and Measurement
¶ Circulating Biomarkers
- C-reactive protein (CRP): Acute-phase protein and inflammation marker
- Interleukin-6 (IL-6): Multi-functional inflammatory cytokine
- Tumor necrosis factor-α (TNF-α): Pro-inflammatory cytokine
- Fibrinogen: Coagulation protein and inflammatory marker
- Erythrocyte sedimentation rate (ESR): Non-specific inflammation indicator
¶ Advanced Inflammatory Panels
- Multi-cytokine arrays: Comprehensive inflammatory mediator profiling
- Chemokine measurements: Cell recruitment signal assessment
- Complement factors: Innate immune system activation markers
- Adhesion molecules: Endothelial activation and leukocyte binding
- Matrix metalloproteinases: Tissue remodeling enzyme levels
¶ Cellular Assays
- Flow cytometry: Inflammatory cell phenotyping and activation status
- Ex vivo stimulation: Cellular inflammatory response capacity
- Phagocytosis assays: Immune cell clearance function
- Oxidative burst: Neutrophil and macrophage ROS production
- Cytokine production: Cellular inflammatory mediator secretion
¶ Imaging Techniques
- PET imaging: Microglial activation and tissue inflammation
- MRI: Tissue inflammation and blood-brain barrier integrity
- Ultrasound: Vascular inflammation and atherosclerotic plaques
- Optical coherence tomography: Retinal inflammation assessment
- Infrared thermography: Tissue inflammation heat detection
¶ Therapeutic Interventions
¶ Anti-inflammatory Medications
- Non-steroidal anti-inflammatory drugs (NSAIDs): COX enzyme inhibition
- Corticosteroids: Broad-spectrum anti-inflammatory effects
- Disease-modifying antirheumatic drugs (DMARDs): Methotrexate, sulfasalazine
- Biologics: TNF-α, IL-1, IL-6, and other cytokine inhibitors
- JAK inhibitors: Janus kinase pathway blockers
¶ Natural Anti-inflammatory Compounds
- Omega-3 fatty acids: EPA and DHA anti-inflammatory effects
- Curcumin: Turmeric-derived NF-κB inhibitor
- Resveratrol: Polyphenol with anti-inflammatory properties
- Green tea polyphenols: EGCG and catechin anti-inflammatory effects
- Boswellia: Frankincense-derived anti-inflammatory compounds
¶ Lifestyle Interventions
- Regular exercise: Anti-inflammatory myokine production
- Mediterranean diet: Anti-inflammatory nutrition pattern
- Weight loss: Reduced adipose tissue inflammation
- Stress management: Cortisol regulation and inflammation reduction
- Adequate sleep: Circadian rhythm and inflammatory balance
¶ Emerging Therapies
- Senolytic drugs: Senescent cell elimination and SASP reduction
- Autophagy enhancers: Cellular cleanup and inflammation reduction
- Microbiome modulation: Gut bacteria anti-inflammatory effects
- Cold therapy: Controlled inflammatory stress and adaptation
- Photobiomodulation: Light therapy anti-inflammatory effects
¶ Research Frontiers
¶ Resolution of Inflammation
- Specialized pro-resolving mediators: Lipoxin, resolvin, and protectin therapy
- Efferocytosis enhancement: Improved dead cell clearance mechanisms
- Regulatory immune cell therapy: Treg and M2 macrophage enhancement
- Cholinergic modulation: Vagal nerve stimulation and anti-inflammatory effects
- Chronotherapy: Circadian timing of anti-inflammatory interventions
¶ Precision Medicine
- Inflammatory profiling: Individual inflammatory signature assessment
- Genetic variants: Polymorphisms affecting inflammatory responses
- Biomarker-guided therapy: Personalized anti-inflammatory treatment selection
- Multi-omics integration: Comprehensive inflammatory network analysis
- Predictive modeling: Risk assessment and intervention timing
¶ Novel Therapeutic Targets
- Inflammasome inhibition: NLRP3 and other inflammasome complex targeting
- DAMP neutralization: Damage signal scavenging and inhibition
- Metabolic reprogramming: Immune cell metabolism modification
- Epigenetic modulation: Chromatin-mediated inflammatory gene control
- Extracellular vesicle therapy: Anti-inflammatory exosome treatment
¶ Technology Integration
- Nanotechnology: Targeted anti-inflammatory drug delivery
- Biosensors: Real-time inflammation monitoring devices
- Artificial intelligence: Pattern recognition in inflammatory diseases
- Organ-on-chip: Inflammatory disease modeling and drug testing
- Telemedicine: Remote inflammatory disease monitoring and management
¶ Lifestyle and Environmental Factors
¶ Pro-inflammatory Factors
- Processed foods: High-fat, high-sugar, and trans-fat diets
- Sedentary lifestyle: Lack of physical activity and muscle disuse
- Chronic stress: Persistent psychological and physiological stress
- Poor sleep: Sleep deprivation and circadian disruption
- Environmental toxins: Air pollution, heavy metals, and chemicals
¶ Anti-inflammatory Lifestyle
- Whole food diet: Fruits, vegetables, whole grains, and lean proteins
- Regular physical activity: Aerobic exercise and resistance training
- Stress reduction: Meditation, yoga, and relaxation techniques
- Quality sleep: 7-9 hours of restorative sleep nightly
- Social connections: Strong relationships and community involvement
¶ Environmental Considerations
- Air quality: Pollution exposure and respiratory inflammation
- Water quality: Contaminant exposure and systemic inflammation
- Occupational hazards: Workplace toxin and pathogen exposure
- Geographic factors: Climate, altitude, and environmental stress
- Socioeconomic status: Access to healthcare and healthy lifestyle resources
¶ Clinical Assessment and Management
¶ Diagnostic Approach
- Clinical history: Symptom patterns and disease associations
- Physical examination: Signs of systemic inflammation
- Laboratory testing: Inflammatory marker measurement panels
- Imaging studies: Tissue inflammation visualization
- Functional assessments: Organ system performance evaluation
¶ Treatment Strategies
- Risk stratification: Individual inflammatory risk assessment
- Multi-modal intervention: Combined lifestyle and pharmacological approaches
- Monitoring protocols: Regular inflammatory marker tracking
- Side effect management: Anti-inflammatory therapy safety monitoring
- Outcome assessment: Treatment effectiveness evaluation
¶ Prevention Approaches
- Primary prevention: Inflammatory disease risk reduction
- Secondary prevention: Early intervention in inflammatory conditions
- Tertiary prevention: Complication prevention in established disease
- Population health: Community-based inflammatory disease prevention
- Health education: Public awareness and lifestyle modification
¶ Measurement in Clinical Practice
¶ Routine Biomarkers
- High-sensitivity C-reactive protein: Cardiovascular risk assessment
- Complete blood count: White blood cell and inflammatory indices
- Erythrocyte sedimentation rate: General inflammation screening
- Fibrinogen: Coagulation and inflammatory marker
- Albumin: Negative acute-phase protein and nutritional status
¶ Specialized Testing
- Cytokine panels: Multi-analyte inflammatory mediator measurement
- Autoantibody screening: Autoimmune disease detection
- Complement levels: Innate immune system activation assessment
- Cellular immunophenotyping: Immune cell subset analysis
- Functional immune assays: Cellular response capacity testing
¶ Videos and Educational Resources
¶ Scientific Lectures
- Inflammaging - Claudio Franceschi - Inflammation and aging pioneer
- Resolution of Inflammation - Charles Serhan - Pro-resolving mediator discovery
- Chronic Inflammation - Peter Libby - Cardiovascular inflammation expert
¶ Educational Content
- What is Inflammation? - Khan Academy - Basic inflammatory concepts
- Chronic Disease and Inflammation - Harvard - Disease mechanisms
- Anti-inflammatory Diet - Mayo Clinic - Nutritional approaches
¶ References
-
López-Otín, C., et al. (2023). "Hallmarks of aging: An expanding universe." Cell, 186(2), 243-278. PubMed
-
Franceschi, C., et al. (2018). "Inflammaging: a new immune-metabolic viewpoint for age-related diseases." Nature Reviews Endocrinology, 14(10), 576-590. PubMed
-
Ferrucci, L., & Fabbri, E. (2018). "Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty." Nature Reviews Cardiology, 15(9), 505-522. PubMed
-
Furman, D., et al. (2019). "Chronic inflammation in the etiology of disease across the life span." Nature Medicine, 25(12), 1822-1832. PubMed
-
Libby, P. (2021). "The changing landscape of atherosclerosis." Nature, 592(7855), 524-533. PubMed
-
Serhan, C. N., et al. (2018). "Treating inflammation and infection in the 21st century: new hints from decoding resolution mechanisms and pathways." FASEB Journal, 31(4), 1273-1288. PubMed
Part of the Hallmarks of Aging series