¶ Sunlight and Health: Mechanisms, Risks, and Longevity
Sunlight exposure is a potent environmental regulator of human physiology, acting as a "double-edged sword" with significant implications for healthspan and lifespan. While excessive exposure is a validated carcinogen and the primary driver of cutaneous aging, complete avoidance has been identified as a major risk factor for all-cause mortality, comparable in magnitude to smoking.
Physiologically, sunlight drives the cutaneous synthesis of Vitamin D3, releases bioactive nitric oxide (NO) into systemic circulation, and entrains the circadian rhythm via retinal signaling. Epidemiological data suggests that for the general population, the cardiovascular and metabolic benefits of moderate sun exposure may outweigh the risks of cutaneous malignancy. Modern clinical guidance is shifting from universal avoidance toward risk-stratified protocols based on skin phenotype (Fitzpatrick type) and UV index.
¶ Mechanisms of Action
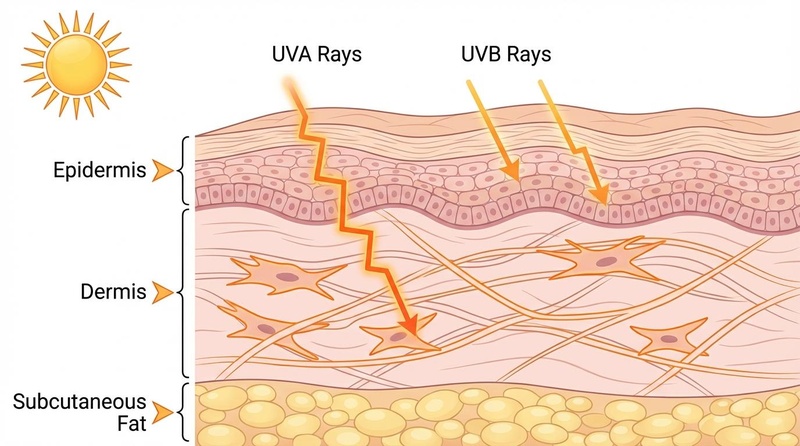
Solar radiation reaching the Earth's surface comprises ultraviolet (UV), visible, and infrared radiation. Each spectrum interacts with specific chromophores in the human body to elicit distinct biological responses.
¶ Vitamin D Synthesis (UVB)
The most well-characterized benefit of sunlight is the cutaneous synthesis of Vitamin D, a secosteroid hormone essential for musculoskeletal health and immune function.
- Pathway: Ultraviolet B (UVB) radiation (290–315 nm) penetrates the epidermis and photolyzes 7-dehydrocholesterol (7-DHC) into previtamin D3. This unstable intermediate thermally isomerizes into vitamin D3 (cholecalciferol), which enters the circulation[1][2].
- Optimal Conditions: UVB radiation is easily scattered by the atmosphere. Synthesis is maximized when the solar elevation angle is high (near solar noon). In early morning or late afternoon, the longer atmospheric path filters out most UVB, halting Vitamin D production while still transmitting UVA[3].
- Limitations: Synthesis is self-limiting (excess exposure degrades previtamin D3 into inactive metabolites), preventing toxicity from sun exposure alone. Darker skin (higher melanin) requires significantly longer exposure (3-6x) to generate equivalent Vitamin D compared to pale skin[2:1].
¶ Nitric Oxide Release and Blood Pressure (UVA)
Research indicates a rapid, hypotensive effect of sunlight independent of Vitamin D, mediated by Ultraviolet A (UVA) radiation.
- Mechanism: The skin stores large reserves of nitrogen oxides (nitrate/nitrite). Exposure to UVA radiation (315–400 nm) photochemically reduces these stores to bioactive Nitric Oxide (NO), which is released into the systemic circulation[4].
- Cardiovascular Impact: NO induces systemic arterial vasodilation, leading to a significant reduction in both systolic and diastolic blood pressure. This mechanism helps explain the observed latitudinal gradient in hypertension and cardiovascular mortality (lower rates in sunnier regions), which persists even after adjusting for temperature[5][6].
¶ Circadian Entrainment and Neurobiology
Sunlight is the primary zeitgeber (time-giver) for the human circadian clock, influencing sleep, metabolism, and mood.
- SCN Signaling: Intrinsically photosensitive retinal ganglion cells (ipRGCs) detect high-intensity blue light (~480 nm) present in sunlight. They project directly to the suprachiasmatic nucleus (SCN) of the hypothalamus to suppress melatonin production and stimulate cortisol release, anchoring the sleep-wake cycle[7].
- Mood and Serotonin: Sunlight exposure increases brain serotonin turnover. Insufficient exposure is the primary pathophysiology behind Seasonal Affective Disorder (SAD).
- -Endorphin Release: UV exposure stimulates epidermal keratinocytes to express pro-opiomelanocortin (POMC), which is cleaved into melanin (for tanning) and -endorphin. In animal models, this endogenous opioid release promotes "sun-seeking" behavior and can induce withdrawal symptoms upon blockade, suggesting a biological basis for the desire to sunbathe[8].
¶ Mortality and Longevity Evidence
While the carcinogenic risks of UV radiation are well-established, large-scale epidemiological studies have uncovered a "mortality paradox" where sun avoidance correlates with shorter lifespans.
¶ The MISS Cohort Study
The Melanoma in Southern Sweden (MISS) cohort followed approximately 30,000 women for 20 years to evaluate the relationship between sun exposure habits and mortality.
- All-Cause Mortality: The study found an inverse relationship between sun exposure and all-cause mortality. Women with the highest sun exposure habits had a significantly lower mortality rate than those with the lowest exposure[9].
- Comparison to Smoking: In a competing risk analysis, non-smokers who avoided the sun had a life expectancy similar to smokers in the highest sun-exposure group. The authors concluded that "avoidance of sun exposure is a risk factor for death of a similar magnitude as smoking," primarily due to increased cardiovascular disease risk in avoiders[9:1][10].
¶ The Cardiovascular Trade-off
The longevity benefit observed in sun-seekers is driven largely by a reduction in cardiovascular disease (CVD) and non-cancer/non-CVD death. Since CVD accounts for a much larger proportion of global mortality than skin cancer, the net effect of moderate sun exposure on population-level longevity appears positive[11].
- Cancer Survival: Paradoxically, some studies indicate that patients diagnosed with melanoma who have a history of high sun exposure have better survival rates than those with low exposure, potentially due to superior Vitamin D status or less aggressive tumor biology associated with chronic exposure (as opposed to intermittent burning)[12].
¶ Risks of Exposure
Sunlight is a complete carcinogen and the primary external cause of skin aging. Understanding these risks is crucial for developing safe protocols.
¶ UV-Induced DNA Damage
- UVB: Directly absorbed by DNA, causing the formation of cyclobutane pyrimidine dimers (CPDs) and 6-4 photoproducts. If unrepaired by nucleotide excision repair (NER), these lesions lead to "UV-signature" mutations (CT transitions)[13].
- UVA: Generates reactive oxygen species (ROS) that cause oxidative DNA damage (e.g., 8-oxo-guanine). Recent evidence suggests UVA can also induce CPDs via "dark" chemical excitation pathways that continue hours after exposure[14].
¶ Photoaging (Dermatoheliosis)
Chronic sun exposure is responsible for up to 80% of visible facial aging.
- Mechanism: UV-induced ROS activate AP-1 transcription factors, which upregulate Matrix Metalloproteinases (MMPs). These enzymes degrade collagen and elastin fibers in the dermis, leading to solar elastosis (accumulation of dystrophic elastic tissue), deep wrinkles, and laxity[15].
¶ Skin Cancer Risk
- Melanoma: The deadliest form of skin cancer is strongly associated with intermittent, intense exposure (sunburns), particularly during childhood and adolescence. Interestingly, chronic moderate exposure (e.g., in outdoor workers) is often associated with a lower risk of melanoma on sun-exposed sites, likely due to photo-adaptation (tanning/thickening)[16].
- Non-Melanoma Skin Cancer (NMSC): Squamous Cell Carcinoma (SCC) is directly linked to cumulative lifetime UV dose. Basal Cell Carcinoma (BCC) is associated with both intermittent and cumulative exposure[16:1].
¶ Clinical Guidelines and Protocols
Guidelines are evolving from a "zero tolerance" approach toward nuanced risk stratification that balances the needs for Vitamin D/NO against carcinogenic risks.
¶ Risk Stratification (Fitzpatrick Scale)
Protocols must be customized based on the Fitzpatrick Skin Phototype:
| Type | Phenotype | Burn/Tan Response | Risk Profile | Recommendation |
|---|---|---|---|---|
| I-II | Pale white, blue/green eyes, red/blonde hair. | Always burns, never tans. | High melanoma/NMSC risk. Low Vit D threshold. | Strict protection. Supplement Vit D. Limit exposure to <10 mins. |
| III-IV | White to light brown. | Burns moderately, tans gradually. | Moderate risk. | Moderate exposure (10-20 mins) permitted. Protect when UV Index 3. |
| V-VI | Dark brown to black. | Rarely burns, tans profusely. | Low skin cancer risk. High Vit D deficiency risk. | Exposure encouraged. Natural melanin provides SPF ~13. |
¶ "Safe Sun" Practices
- Avoid Erythema (Burning): The cardinal rule is to never burn. Erythema indicates DNA damage has exceeded repair capacity.
- Gradual Acclimatization: Slowly building exposure allows the skin to thicken (acanthosis) and synthesize melanin, providing natural protection (photo-adaptation).
- Timing (The Window Debate):
- Standard Dermatology View: Avoid peak sun (10 AM – 2 PM) to minimize total UV load.
- Photobiology View: Midday exposure provides the highest ratio of UVB (Vit D) to UVA (Aging). Short exposures (10-15 mins) at solar noon are most efficient for Vitamin D synthesis. Morning/evening sun provides almost exclusively UVA, contributing to aging without Vitamin D benefits[3:1].
- Protection: Physical barriers (clothing, hats) are preferred. Broad-spectrum sunscreen is essential for extended exposures but blocks Vitamin D synthesis if applied immediately and thoroughly.
¶ References
Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266-281. ↩︎
Bikle DD. Vitamin D metabolism, mechanism of action, and clinical applications. Chem Biol. 2014;21(3):319-329. ↩︎ ↩︎
Webb AR, Engelsen O. Calculated ultraviolet exposure levels for a healthy vitamin D status. Photochem Photobiol. 2006;82(6):1697-1703. ↩︎ ↩︎
Opländer C, Volkmar CM, Paunel-Görgülü A, et al. Whole body UVA irradiation lowers systemic blood pressure by release of nitric oxide from intracutaneous photolabile nitric oxide derivates. Circ Res. 2009;105(10):1031-1040. ↩︎
Weller RB. The health benefits of UV radiation exposure through vitamin D production or non-vitamin D pathways. Photochem Photobiol Sci. 2017;16(3):374-380. ↩︎
Liu D, FernandezBO, Hamilton A, et al. UVA irradiation of human skin vasodilates arterial vasculature and lowers blood pressure independently of nitric oxide synthase. J Invest Dermatol. 2014;134(7):1839-1846. ↩︎
Berson DM, Dunn FA, Takao M. Phototransduction by retinal ganglion cells that set the circadian clock. Science. 2002;295(5557):1070-1073. ↩︎
Fell GL, Robinson KC, Mao J, Woolf CJ, Fisher DE. Skin -endorphin mediates addiction to UV light. Cell. 2014;157(7):1527-1534. ↩︎
Lindqvist PG, Epstein E, Landin-Olsson M, et al. Avoidance of sun exposure is a risk factor for all-cause mortality: results from the Melanoma in Southern Sweden cohort. J Intern Med. 2014;276(1):77-86. ↩︎ ↩︎
Lindqvist PG, Epstein E, Nielsen K, et al. Avoidance of sun exposure as a risk factor for major causes of death: a competing risk analysis of the Melanoma in Southern Sweden cohort. J Intern Med. 2016;280(4):375-387. ↩︎
Alfredsson L, Armstrong BK, Butterfield DA, et al. Insufficient Sun Exposure Has Become a Real Public Health Problem. Int J Environ Res Public Health. 2020;17(14):5014. ↩︎
Berwick M, Armstrong BK, Ben-Porat L, et al. Sun exposure and mortality from melanoma. J Natl Cancer Inst. 2005;97(3):195-199. ↩︎
Mouret S, Baudouin C, Charveron M, Favier A, Cadet J, Douki T. Cyclobutane pyrimidine dimers are predominant DNA lesions in whole human skin exposed to UVA radiation. Proc Natl Acad Sci U S A. 2006;103(37):13765-13770. ↩︎
Premi S, Wallisch S, Mano CM, et al. Photochemistry. Chemiexcitation of melanin derivatives induces DNA photoproducts long after UV exposure. Science. 2015;347(6224):842-847. ↩︎
Fisher GJ, Kang S, Varani J, et al. Mechanisms of photoaging and chronological skin aging. Arch Dermatol. 2002;138(11):1462-1470. ↩︎
Gandini S, Sera F, Cattaruzza MS, et al. Meta-analysis of risk factors for cutaneous melanoma: II. Sun exposure. Eur J Cancer. 2005;41(1):45-60. ↩︎ ↩︎